While many patients are treated beyond progression, the magnitude and duration of clinical benefit in these patients have not been fully quantified. This study assessed the efficacy of pembrolizumab in patients who continued treatment beyond disease progression, demonstrating that it provided meaningful benefits for select patients across various cancer types, including melanoma, non-small cell lung cancer, renal cell carcinoma and urothelial carcinoma.
INTRODUCTION
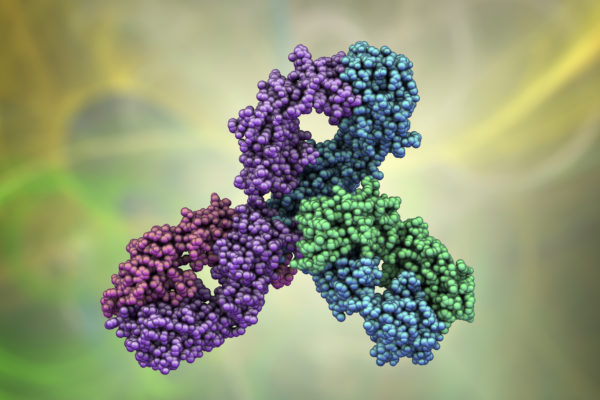
The Response Evaluation Criteria in Solid Tumours (RECIST) guidelines were originally developed and refined (RECIST version 1.1 [v1.1]) to assess tumour response to cytotoxic agents. However, RECIST guidelines may not accurately assess response to immunotherapy, and some patients on immunotherapy show apparent progressive disease (PD) under RECIST v1.1, even though certain lesions remain stable or shrink. This suggests ongoing treatment efficacy for specific lesions. To address this issue, clinical trials sometimes let patients continue immunotherapy after initial progression. This study examined the effectiveness of pembrolizumab in patients who continued treatment beyond RECIST v1.1-defined progression. These findings help assess the potential of combining novel therapies with PD-1 inhibitors in patients with PD-1 inhibitor-refractory disease.
METHODS
This analysis includes data from patients who were treated with pembrolizumab monotherapy in several clinical trials: KEYNOTE-001 (melanoma and non-small cell lung cancer [NSCLC]), KEYNOTE-059 (gastric cancer [GC]), KEYNOTE-048 (head and neck squamous cell carcinoma [HNSCC]), KEYNOTE-427 (clear-cell renal cell carcinoma [ccRCC]), KEYNOTE-052, and KEYNOTE-361 (urothelial carcinoma [UC]). Eligible patients had to have received at least one dose of pembrolizumab beyond PD per RECIST v1.1, received at least two doses of pembrolizumab by the time of PD diagnosis, had PD confirmed (per RECIST v1.1) at least four weeks after PD was first documented, and experienced PD less than 12 weeks after the last dose of pembrolizumab. All data were analysed using MATLAB 2021a.
STUDY FINDINGS
Data from 799 patients with melanoma (n = 176), NSCLC (n = 146), GC (n = 87), HNSCC (n = 112), ccRCC (n = 51), and UC (n = 227) were analysed. These patients received pembrolizumab beyond confirmed progression per RECIST v1.1. Among patients with melanoma, 24% had a clinically meaningful reduction (R≥30%) in the sum of target lesion diameters in the post-progression period. In patients with NSCLC and GC, this percentage was 11.6% and 12.6%, respectively. Most patients (≥90%) displayed at least one stable or shrinking lesion in these cancers. The proportion of patients with R≥30% in the sum of target lesion diameters in the post-progression period ranged from 9% to 16% for other cancer types (8.9% HNSCC, 15.7% ccRCC, and 13.2% UC). Moreover, a significant portion of patients across these cancers displayed stable target lesion dynamics during the post-progression period. Specifically, this proportion was 64.8% of patients with melanoma, 72.6% in NSCLC, 69.0% in GC, 75.9% in HNSCC, 72.5% in ccRCC and 75.3% in UC.
The results of this study provide a baseline expectation per tumour type in patients treated with PD-1 inhibitor therapy beyond PD and confirm that most tumour sites do not demonstrate radiographic evidence of resistance at the time of progression. These data may facilitate a more accurate assessment of the responses observed with novel therapies combined with PD-1 inhibitor therapy in clinical studies without historical controls, refining our understanding of ICI resistance biology.1
REFERENCE