The importance of long non-coding RNAs (lncRNAs) in the adaptive immunity against cancer, through mediating the functional state of immunological cells, routes and genes, has been known for some time now. However, the possible association of lncRNA with clinical outcomes of immunotherapy in cancer treatments was not yet explored.
A newly published study by dr. Tunfang Yu and colleagues showed that classifying lncRNAs of cancer patients can help predict clinical outcomes such as overall survival (OS) and objective response rate (ORR) when they are treated with immunotherapy.1
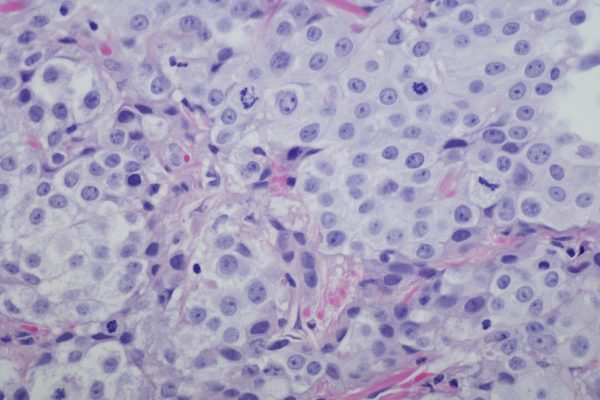
The phase II-study included 348 bladder cancer patients from the IMvigor210-study and 71 melanoma patients from the Cancer Genome Atlas program (TCGA).2,3 These patients all received immunotherapy; the bladder cancer patients atezolizumab and the melanoma patients different immunotherapeutic treatments such as anti-PD-1, CTLA4 or a cytokine tumour vaccine.
While analysing the bladder cancer patients from the IMvigor210-study, it was possible to distinguish four different groups with a significant difference in OS (p=0.002). These groups were distinguished by possessing a functional or non-functional immune class, as well determing whether the amount of cytotoxic T-lymphocyte(CTL)-infiltration was high or low.
Based on the clinical immuno-subtype, the patients were divided into 2 different groups with a significant survival difference (HR: 0.65, 95% CI: 0.50-0.84, p=0.001). Surprisingly, patients with a longer survival showed a lower expression of immune cells, immune checkpoints and human leukocyte antigen, compared to patients with a shorter OS.
The researchers then crafted the hypothesis that the immune cells from patients with a shorter OS were in a non-functional state. The lncRNA-profile of this group was therefore classified as the ‘immune-nonfunctional class’ and the lncRNA-profile of the high OS patients as ‘immune-functional class’.
After this, the bladder cancer patients were further divided, based on the amount of CTL-infiltration. Patients with a functional immune response and a high CTL-infiltration showed a higher expression of immune molecules, compared to patients within the immune-functional class with low CTL-infiltration. The same was true for patients in the nonfunctional immune class. These 4 groups showed distinct gene expression patterns.
Patients who were both in the immune-functional class and demonstrated high CTL-infiltration showed the highest advantage in OS as well as ORR. Patients with low CTL-infiltration and who had a lncRNAs profile in the immune-nonfunctional class showed the worst outcomes in these measures.
Knowledge on these 4 groups can be used in understanding the mechanisms used by cancer cells to escape immunologic destruction, but also in selecting the right patients for immunotherapy. Seeing immunotherapy can cause serious adverse events, and the fact that it is only effective in a specific patient population, makes it important to use biomarkers to select the patients with the highest chance of succeeding on the therapy.
References