Multiple endocrine neoplasia 2 (MEN2) syndrome is an inherited familial disorder that can cause multiple hormone-producing tumours. These tumours develop in glands, organs and tissues that produce hormones, and the excess hormone production can cause symptoms. MEN2 results from germline mutations in the RET proto-oncogene and is transmitted in an autosomal dominant fashion. There are two MEN2 syndromes: MEN2A and MEN2B.
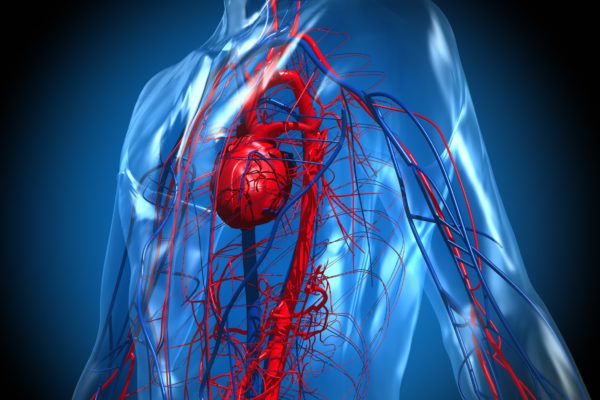
Hormones are chemical messengers that are produced by the endocrine system and that are transported to cells or organs via the blood stream. The pancreas is one of these endocrine organs: it produces the hormone insulin, which regulates blood sugar levels. Other hormone-producing glands are the parathyroid glands, the thymus and the adrenal glands.
Almost all MEN2 patients develop thyroid cancer, and half of the patients also present tumours in the adrenal glands.
MEN2A and MEN2B are different in certain respects:
Half of all patients will develop a tumour in the adrenal glands. Of these, 70% will get tumours in both glands. The tumour will always occur in the adrenal medulla and is also known as pheochromocytoma. In MEN2A patients, this is almost always a non-malignant growth. This type of tumour causes excess production of adrenalin and noradrenalin. Around one in every five MEN2A patients will develop tumours in the parathyroid gland, 70% of whom will develop tumours in both glands. Usually non-malignant, these tumours cause excess production of parathyroid hormones, a condition known as hyperparathyroidism.
Almost all MEN2 patients will develop tumours in the thyroid glands. These tumours originate in the C cells of the thyroid and start off as benign. These tumours almost always turn malignant, after when they are known as medullar thyroid carcinoma. These are slow-growing tumours that can take years before they make their presence known to the patient. MEN2 is a familial hereditary condition, but may also be caused by spontaneous gene mutation.
The nature of symptoms in patients with MEN2 depends on the location of the tumour. In MEN2A patients, tumours can develop throughout their lives. In MEN2B patients, symptoms can occur at a very young age.
Patients with adrenal gland cancer can present:
The cause of the MEN2 syndrome is found in the patients’ genes. Specifically, it involves a mutation in the RET gene, which is located in chromosome 10. The RET gene is involved in the production of the protein RET. This protein triggers mitosis in cells, but the mutation causes uncontrolled mitosis, leading to the formation of a tumour. This is why this particular gene is known as the ‘proto-onco gene’. There are numerous mutations possible in the RET gene that can lead to the MEN2 syndrome. These mutations determine at which age the patient develops thyroid cancer.
An endocrinologist establishes a diagnosis based on the symptoms a patient presents and will also inquire whether MEN2 occurs in the patient’s family. To determine whether someone has a genetic disposition towards MEN2, genealogical and DNA research are necessary. In the genealogical research, the occurrence of MEN2 in the patient’s family is established. The DNA research determines whether the MEN2-related mutations are present.
If research shows that the syndrome is present in a patient, or that there is a large likelihood, the GP will recommend regular check-ups so that tumours can be detected at an early stage. Early diagnosis greatly improves the outcome. Since developing thyroid cancer in MEN2 patients is almost a certainty, preventative removal of the thyroids, often during childhood, is a common strategy. If the diagnosis is made at a later age, thyroid removal is still an option. In case of MEN2B, the thyroids are removed as early as possible, sometimes even during the first year.
People who have been diagnosed with MEN2 or with a large probability of developing the disease can have regular check-ups. Besides physical examination and blood tests, CT scans, MRI scans and ultrasounds are also common.
If one or more tumours are found during examination, the oncology team will devise a treatment strategy. The exact treatment is determined by the type of cancer, its location and its stage.
In case of a parathyroid tumour, a surgeon will remove the parathyroid glands partly or in full. Should all four glands need to be removed, then a small tumour-free part of one of the glands can be transplanted into the lower arm. When deemed necessary, the surgeon may also opt to remove the thymus.