In the primary analysis of the CLEAR study, lenvatinib plus pembrolizumab significantly improved progression-free survival (PFS) and overall survival (OS) vs. sunitinib in patients with advanced renal cell carcinoma. With 7 months of additional follow-up, the updated results of this trial solidify the PFS and OS superiority of lenvatinib plus pembrolizumab over sunitinib in this setting. These results were recently published in The Lancet Oncology.
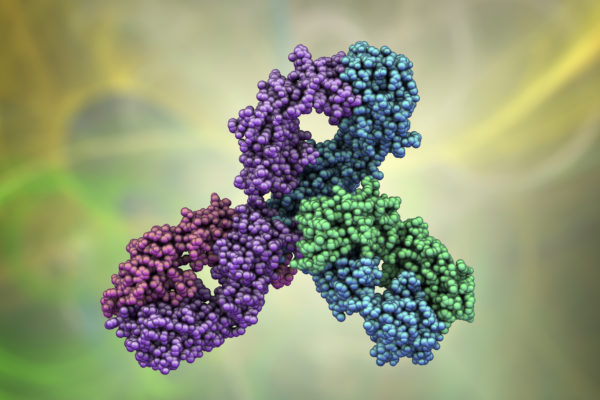
Treatment with immune-checkpoint inhibitors, either as a dual type combination or in combination with kinase inhibitors, provides better outcomes than sunitinib for patients with metastatic renal cell carcinoma (rCC). These patients can also benefit from the treatment combination of lenvatinib, an antiangiogenic agent, and pembrolizumab, an anti-programmed cell death1 (PD-1) monoclonal antibody. Based on these observations, the phase 3 CLEAR trial compared the efficacy and safety of lenvatinib in combination with the mTOR kinase inhibitor everolimus or pembrolizumab vs. sunitinib alone in first-line treatment of advanced rCC. In the primary analysis, lenvatinib plus pembrolizumab significantly improved progression-free survival (PFS) and overall survival (OS) vs. sunitinib. This protocol-prespecified analysis reported the updated survival results after 7 months of additional follow-up, for the lenvatinib plus pembrolizumab and sunitinib arms.
The phase 3 CLEAR study included patients with clear-cell advanced renal cell carcinoma (ccRCC) who had not received any systemic anticancer therapy for RCC, coming from 200 hospitals and cancer centres across 20 countries. In total, 1,069 patients were randomly assigned (1:1:1) to receive lenvatinib plus pembrolizumab (n=355), lenvatinib plus everolimus (n=357), or sunitinib (n=357). The primary endpoint was progression-free survival (PFS). This protocol-prespecified updated analysis reports the extended follow-up analyses for PFS and OS. No safety analyses were done during this follow-up.
The median follow-up for PFS was 27.8 months in the lenvatinib plus pembrolizumab group and 19.4 months in the sunitinib group. For OS, follow-up was 33.7 and 33.4 months, respectively. In this study, lenvatinib plus pembrolizumab resulted in a statistically significant improvement in PFS (23.3 vs. 9.2 months) compared to sunitinib (HR[95%CI]: 0.42 [0.34-0.52]). Although the median OS was not reached by any of the arms, the hazard ratio favoured lenvatinib plus pembrolizumab HR[95%CI]: 0.72 [95%CI: 0.55-0.93]).
In this study, the efficacy benefits of lenvatinib plus pembrolizumab over sunitinib were durable and clinically meaningful with extended follow-up. These results support the use of lenvatinib plus pembrolizumab as a first-line therapy for patients with advanced rCC.
Reference